
When there’s a problem in the brain, it pays to be precise — every millimeter counts with something like a tumor or blocked artery. But it can be extremely difficult to understand the exact shape and size of these things, which makes them difficult to diagnose and treat, as well. But 3D printing a replica of the growth or damage may make doctors better able to do so.
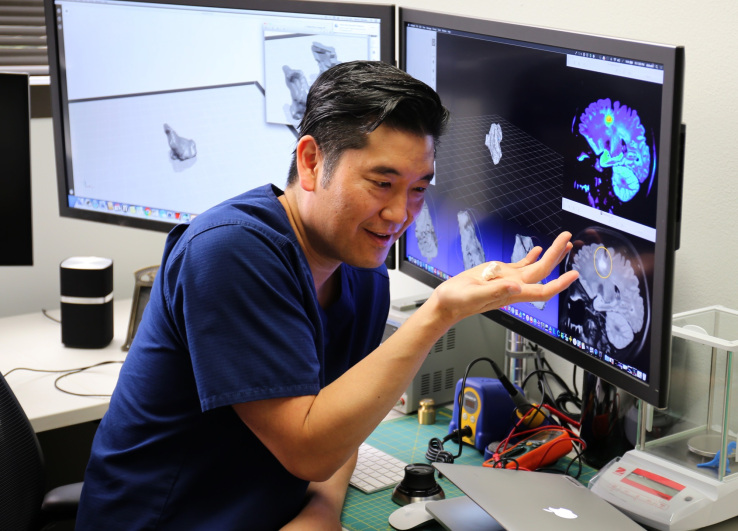
That’s the suggestion made by Dr. Darin Okuda (above), who recently published some work showing the effectiveness of this printing method in diagnosing and understanding brain lesions found in multiple sclerosis patients.
Okuda’s team analyzed MRI scans of MS-affected brains and printed exact copies of the lesions, or damaged areas, detected in them. These were given to people who would normally have just used 2D images or a 3D reconstruction on a screen to diagnose or monitor this type of thing.

“What you see on plain 2-dimensional views does not give one a clear understanding as to the true shape of the lesion itself,” Okuda told me. “By studying lesions in 3D, we are looking at these findings in an entirely different way, assessing their shape and surface characteristics.”
They identified a number of features that distinguish MS lesions from other types of brain damage, such as asymmetry and complex surface structures. These weren’t always obvious from scans and the transition to 3D let the participants more easily perceive them.
“Prior to the release of our work, we were describing multiple sclerosis lesions incorrectly,” said Okuda. “Lesions from MS are still described as being ‘ovoid’ in shape and ‘well circumscribed’ in character. Based on our 3D work, we know that this is not the case. We were amazed at the complexity of MS lesions and would argue that conventional terms previously used in our field may not be accurate after a review in physical 3D form.”
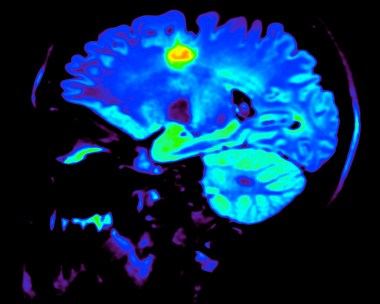
A scan like this one only gives a limited idea of the shape of the lesion
Knowing this could be the difference between a correct and incorrect diagnosis, and 3D printing something is cheap and relatively quick. One could even print it out larger than life to get a better idea of its shape. The objects could also help patients understand the damage and how it can be treated, or see the results of that treatment outside of obscure visualizations and diagrams.
It may seem to you, as it did to me, that 3D visualization of 3D structures in the brain is a pretty obvious thing to do. But technology is in some ways very slow to arrive in medical fields, and 3D visualization in this type of clinical situation is no exception.
“It’s not as widespread as you think,” Okuda explained when I suggested that 3D visualization was prevalent in some ways already. “Other brain lesion imaging work that you have seen likely represents efforts related to CT scans or combination CT/MRI work for pre-surgical planning (with limited surface and shape resolution). Although it may seem intuitive, we do not use 3D imaging in the diagnosis and management of malignant brain tumors.”

Dr. Okuda showing off his lesion collection
Room to expand the technique, then, perhaps.
The next phase for Okuda and his team is, first, to make a VR platform for patients to use when 3D printing is not practical. And because this is an optimal use case for machine learning, development of deep learning systems is also underway. It may be that certain shapes or features could predict clinical outcomes or otherwise figure into the prognosis.
Okuda et al. published their work in a recent volume of the Journal of Neuroimaging.

